Breastfeeding is a learning experience for both mother and baby. Here are some tips to get you off to a good start.
In this fact sheet, you’ll learn how to lay a strong foundation for breastfeeding.
The early days
Your body produces certain hormones during pregnancy to prepare your breasts for breastfeeding. As soon as you give birth, your breasts begin secreting colostrum. Colostrum is your baby’s first milk. It is yellowish-orange in colour and extremely rich in vitamins and minerals. The white blood cells and antibodies in colostrum help protect newborns from infection. Colostrum also helps evacuate any waste that has built up in the intestine during pregnancy.
Breastfeeding can be challenging at first. Some mothers and babies need extra time to get the hang of it. The best approach is to trust yourself and follow your instincts. If you have any concerns, be sure to contact a breastfeeding support group.
It’s important to take advantage of your newborn’s first period of alertness to kick off breastfeeding. This is usually within two hours of birth. When placed on their mothers skin-to-skin, many babies will latch on properly or touch or lick the breast, stimulating milk production.
Some babies can be very sleepy after they are born and are not ready to drink. If this is the case, continue skin-to-skin contact and try breastfeeding a little later. Close contact with their mother triggers certain reflexes in a baby. These reflexes can help babies latch onto the breast properly.
Breasts produce very small amounts of colostrum. This is because newborns have tiny stomachs and only ingest a few millilitres during their first few feedings. It is normal for your baby to suckle often while they are learning to breastfeed. These small, frequent feedings prompt your body to produce more milk.
Sometime between the second and fifth day, colostrum is replaced by a whiter, more translucent milk that’s equally rich and nutritious. Your milk production will increase rapidly at this point. This process is called milk coming in and will happen even if your baby isn’t breastfeeding.
Afterwards, your breasts will need stimulation to maintain milk production. Milk production is based on the law of supply and demand: the more often the breasts are emptied, the more milk they produce. Conversely, the less they are stimulated, the less they produce.
When breasts become engorged, some mothers may experience a slight increase in body temperature. If you have a fever above 38°C (100.4°F) along with additional symptoms, you should see a doctor. |
As the milk comes in, the breasts can become quite swollen and tight. This is completely normal. In fact, it’s a sign that you’re starting to produce milk, and all the alveoli in your breasts are being activated simultaneously. This discomfort lasts 2 to 3 days.
Frequent day and nighttime feedings during this period (more than 8 times in 24 hours) will help speed up the process, and the frequent emptying will ensure that your breasts don’t become too engorged. This will also ensure that your milk supply can meet your baby’s needs.
During these early days, nursing your baby at the first sign of hunger is recommended. Feeding them before they become too hungry ensures that your baby’s energy needs are met. It’s also the best time for them to learn how to latch.
Download this chart to keep track of how often your baby feeds, their bowel movements, and their urine output.

Babies give several hunger cues: Their eyes move back and forth under closed lids, their mouth starts to suckle, and their arms and legs become active. Next, they open their eyes, bring their hands to their mouth, and turn their head looking for the breast.
It’s best not to wait until your baby cries. Crying is the last sign of hunger and means that your baby is in distress.
Let your baby set the pace and trust their instincts. However, if your baby has been sleeping for a long stretch, you should watch for the slightest sign of waking, then place them skin-to-skin on your chest and offer your breast.
Uterine cramping and breastfeedingOxytocin, a hormone that’s secreted when a baby suckles your breast, is also responsible for uterine contractions during childbirth. This is why women often feel cramping in the first few days of breastfeeding. The cramps are more intense after second and subsequent births due to the larger size of the uterus. These contractions have a purpose: they help the uterus return to its normal size and help prevent hemorrhaging. |
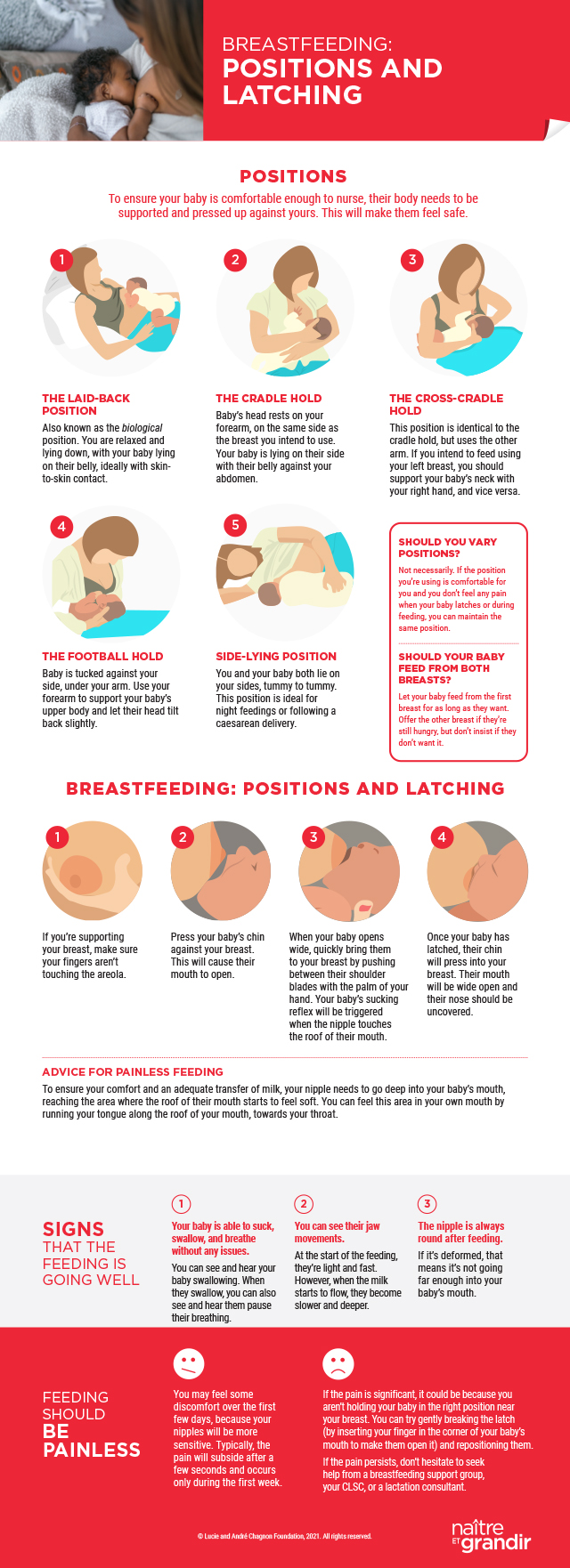
Breastfeeding positions and latching
There are a number of breastfeeding positions to choose from, including the laid-back, cradle, football, and side-lying holds. Ask a nurse or your labour partner to help you experiment with different positions in the first few days, then pick the one that’s most comfortable.
A proper latch is the key to pain-free breastfeeding. However, you may still feel discomfort with a good latch during the first few days because your nipples are more sensitive. This discomfort usually passes in seconds and should only last about a week. Suction can cause increased sensitivity if it is not optimal from the outset.
If the pain persists, even after correcting the latch, we recommend meeting with an IBCLC-certified lactation consultant. Persistent pain is not normal and could indicate a more serious problem.
How long does a feed last?
Feedings will seem long at first. By the time you settle in, get the baby to nurse, burp them, and change their diaper, feedings can easily last 45 minutes or more. That said, as your baby becomes more alert and experienced, feeding sessions will become more efficient and less time-consuming.
Your breast milk also changes over time to adapt to the needs of a growing baby. Its composition varies throughout the day, and even during a feeding. Furthermore, it’s impossible to completely empty a breast; the breast is drained, which in turn stimulates milk production. Therefore, there is no minimum interval between feedings. Your milk will be nutritious no matter how often your baby feeds.
How to know when your baby is hungryThere are a few hunger cues to look out for, and they happen long before your baby starts crying: -
Your baby’s breathing changes, and their eyes, mouth, and face become more active.
-
They start to move their arms and legs, stretch, and bring their hands to their mouth and face.
-
Next the suckling reflexes kick in.
It’s time to feed your baby. If you wait until your baby starts to cry, it will be harder for them to latch on well. |
A few tips to make breastfeeding easier
- At the start of a nursing session, your baby will drink actively and take short breaks. As the feeding progresses, their breaks will become longer, and they may stop suckling. If necessary, use the breast compression technique to get your baby to continue feeding.
-
You can stop breastfeeding once your baby has been actively nursing, their pauses are getting longer and, despite stimulation, they no longer want to drink (i.e., their suckling movements are weaker and shorter). To break the latch, insert your index finger in the corner of your baby’s mouth, between their gums. This will keep them from pinching your nipple as they release your breast.
-
Next, try to get your baby to burp. Place a towel over your shoulder, then hold baby upright against your shoulder for 1 or 2 minutes. Gently rub or pat their back. Walk around slowly while you hold them. You can also hold your baby across your lap, on their stomach, and rub their back, or sit them up on your lap, supporting their chin with one hand and rubbing their back with the other. If your baby doesn’t burp, it’s okay. You can always try again later, even after you put them to bed.
- Offer your other breast if your baby is still hungry. If your baby doesn’t want to feed, but your breast is tight because they haven’t suckled, you can express your milk manually or with a breast pump to ease discomfort. You can store this milk for when you need to be away from home.
The father: An indispensable partner in your breastfeeding journeyGetting your partner involved can help tremendously with breastfeeding. They often provide the encouragement and support you need to get through any difficult moments as you learn to breastfeed. They can help you feel more comfortable during the first few days by bringing you a pillow, a glass of water, or a snack, bringing your baby to you during the night, changing your baby’s diaper after they nurse, etc. They can also help deflect any negative comments from family and friends who are being critical about breastfeeding. In short, partners provide encouragement, support your desire to breastfeed, and help you stay the course. |
Has your baby had enough to drink?
Are you wondering if your little one has had enough to drink? This is a common concern for new mothers. Here are a few clues to guide you:
-
Between the ages of 1 week to 1 month, your baby should wet 6 to 8 diapers a day, and at least one should be soiled (with yellowish, soft stools). After the first month, your baby should continue to wet 6 to 8 diapers daily. Bowel movements may occur less frequently (one stool every 3 to 7 days).
- Their weight is increasing steadily.
-
Your baby is nursing well and often: 8 or more times in 24 hours.
-
You can see them swallow.
-
They look satisfied and relaxed when they finish feeding.
-
Your breasts feel softer after the feeding.
The let-down reflexYou may feel milk being expelled from your breast as you nurse your baby or a few minutes after they start to feed. This is the milk let-down or the “ejection reflex.” For many women, this phenomenon is accompanied by intense thirst and a tingling sensation in the breast, while other women don’t feel it at all. The let-down reflex is triggered by the secretion of oxytocin, a hormone that’s triggered by the baby’s sucking. The alveoli contract and milk is rapidly ejected through the openings on the surface of the nipple (your nipple has anywhere from 4 to 15 of them). In many cases, the other breast will also begin to leak. This flow is very useful for expressing milk manually or with a breast pump. However, fatigue or anxiety can block this reflex. If this happens, it’s important to relax and rest. You may feel the let-down reflex even when your baby is not feeding. For example, some mothers have an ejection reflex when they hear their baby cry or when they think about their baby. Small nursing pads can be a practical solution. These are placed in your bra to soak up leaks. |
How many times a day should you breastfeed?
Infants usually feed more than 8 times in 24 hours. However, not all babies have the same rhythm. There is no “normal” when it comes to the frequency of feedings. Every mother and baby are unique. The golden rule of breastfeeding in the first few weeks is to let your baby drink on demand, without limiting the number or length of feedings. A baby never takes more milk than necessary. They know how much they need.
The most important thing is that your baby latches on properly, sucks effectively, and swallows the milk. As your baby grows, make sure they are getting at least 6 effective feedings a day. Their sucking becomes more efficient over time, and the feedings may become shorter and more spaced out.
That said, keeping track of your baby’s feedings using the breastfeeding chart that some hospitals give to parents after the delivery can give you a better understanding of your baby’s waking, sleeping, and feeding patterns. You may notice that your baby tends to cluster feed, i.e., they feed more often at certain times of the day (like in the evening) and less often at other times. The longer intervals between feedings don’t necessarily fall at night.
Night feeds are important, because the body produces more prolactin at night, which is an essential hormone for milk production. Breast milk also contains more fat at night than it does at other times. For all of these reasons, it’s important not to skip feedings or to bottle feed your baby.
Expressing milk
There are several reasons for expressing milk:
-
To maintain milk production.
-
To relieve an engorged breast.
-
To have breast milk on hand in case you need to be away from your baby.
-
To give a premature or sick baby access to breast milk.
There are several ways to express your breast milk, either manually or with a breast pump. The choice of method depends on the situation, the frequency, how your baby is being fed, i.e., whether or not they are taking the breast, and, of course, your preference. There is no ideal time for expressing milk. Choose the time that suits you best.
It can be harder to stimulate the let-down reflex when you’re expressing milk, especially the first few times. It’s not unusual to collect just a few drops the first few times you do it. Remember that the quantity of milk expressed does not reflect the quantity of milk you’re producing. With a little practice, it will get easier.
An IBCLC-certified lactation consultant can help you figure out how to express your breast milk in a way that works best for you.
When to use a bottleBottles (and pacifiers) should be avoided for the first 6 weeks, whether you want to use them to feed your baby breast milk or commercial infant formula. The suckling mechanism used to breastfeed is different than the one used to drink from a bottle. For example, bottles flow on their own right from the start, whereas your baby needs to suckle for a minute or two before milk will flow freely from the breast. The position of the baby’s tongue and gums on the nipple and areola is also different from the position on the nipple of a bottle. These differences can create confusion and lead to problems such refusing the breast. Introducing a bottle too early may also decrease the effectiveness of breast stimulation, reducing your milk production. If you need to feed your baby something other than breast milk, use a spoon or a small glass in the first few weeks to give them the milk. A soft sippy cup can also be used from the age of 4 months. |
Storing breast milk
Breast milk is at its freshest when given directly from the breast. However, it refrigerates and freezes well when the proper precautions are taken.
| | | |
| 24 hours at 15°C/59°F (in a cooler with an ice pack) | | 6 months (in the freezer of your refrigerator, do not store in the door)
12 months (in a chest freezer) |
| | | |
Breast milk can be thawed in the refrigerator or by immersing the container in a bowl of warm water. Milk should never be thawed in the microwave to avoid burning your baby. The excessive heat of the microwave may also destroy some components of the breast milk.
Once thawed, milk can be kept for 1 hour at room temperature or for 24 hours in the refrigerator if it hasn’t been reheated. It cannot be refrozen.
Warning! These storage times are not cumulative: You cannot keep milk at room temperature for 4 hours, then 8 days in the refrigerator before freezing.
Too much breast milk?If you have surplus breast milk, consider donating to Quebec’s Public Mother’s Milk Bank. The milk bank is managed by Héma-Québec, and gives premature babies under the age of 32 weeks access to pasteurized human milk. Mothers who give birth prematurely often have difficulty producing enough milk to feed their babies.
To give your excess milk, you must be healthy, a non-smoker, and have a baby under the age of 12 months. You must also live in the greater Montreal or Quebec City areas, or within one hour of the drop-off points in Gatineau, Sherbrooke, Saguenay, or Trois-Rivières. For more information, visit Héma-Québec. |
Finding your rhythm
After a few weeks, most mothers start to feel more comfortable, and breastfeeding becomes easier and more enjoyable. A routine starts to take shape. At this point, parents can start to plan their feedings and organize some outings to the park, with family, etc.
The age at which your baby starts to sleep full nights (i.e., 6 hours in a row) depends on their natural rhythm and their temperament. Introducing cereals into their diet will not affect their sleep cycle. Before the age of 6 months, breast milk is the best food for your baby’s needs.
After a few months, you’ll get to know your baby’s breastfeeding habits. Once your baby is 3 months old, their feedings often become shorter and more spaced out. Your baby becomes more vocal about their needs, and will start to ask you to switch breasts when milk flow slows. Avoid comparing yourself to other mothers. Patterns vary greatly from one baby to the next.
As babies grow, they start to become interested in their surroundings, even while nursing. This can lead to some funny situations. Some mothers may need to isolate themselves with their child to get their attention while feeding.
Are you feeling unsure of your ability to breastfeed and thinking about weaning your baby? You may need some help or encouragement. Talk about the situation with your spouse, a friend, or someone at a breastfeeding resource centre. They will surely have useful advice to share, and getting out of the house will do you a lot of good.
Growth spurtsYour baby will experience “growth spurts” at the ages of 2 weeks, 4 to 6 weeks, 3 months, and 6 months. Your baby will want to nurse more often during these periods, sometimes every hour. This causes some mothers to doubt the quality of their milk. But there is no need to worry; your milk production will adapt very quickly to your baby’s needs. Growth spurts last only a few days, but can be very challenging. Get plenty of rest when you can and eat nutritious snacks if you are hungry. |
Things to keep in mind
-
As soon as your baby is born, your breasts produce milk, called colostrum.
-
In the first few days, nursing your baby at the first sign of hunger is recommended.
-
During the first few months, your baby will drink more than 8 times over a 24-hour period.
| Scientific review: Louise Godin, graduate nurse and lactation consultant, IBCLC
Research and copywriting:The Naître et grandir team
Updated: December 2022
|
Photo: iStockphoto/ValuaVitaly
Sources
Please note that hyperlinks to other websites are not updated regularly, and some may have changed since publication. It is therefore possible that a link may not be found. If a link is no longer valid, use search engines to find the relevant information.
- Encyclopedia on Early Childhood Development
This encyclopedia is available online, free of charge. It covers topics dealing with the psychosocial aspect of childhood development from conception to age five and presents the latest scientific knowledge. Key takeaways on each topic are presented in a convenient format and are intended for parents and caregivers. www.child-encyclopedia.com -
Doré, Nicole, and Danielle Le Hénaff. From Tiny Tot to Toddler: A practical guide for parents from pregnancy to age two. Quebec City, Institut national de santé publique du Québec. www.inspq.qc.ca
-
The Nourri-Source Federation. Le Petit Nourri-Source. 7th ed., 2021.
-
The Nourri-Source Federation. This breastfeeding support movement has more than 600 breastfeeding support volunteers. It has been providing support and information to all families since 1982. Nourri-Source offers a variety of pre- and post-natal activities, information on public breastfeeding spaces, and even a telephone support service. Toll-free number: 18669485160. www.nourri-source.org
-
La Leche League Canada. This volunteer organization, affiliated with La Leche League International, is active in more than 60 countries and offers mother-to-mother support as well as informational and educational tools. Visit lllc.ca or call 1866ALLAITER. You can also call the toll-free number, 18006654324, to find someone in your area who can help.
-
La Leche League International. The Womanly Art of Breastfeeding. La Leche League Editions, 2005.
-
Canadian Paediatric Society, Dietitians of Canada, and Health Canada. “Nutrition for Healthy Term Infants.” www.hc-sc.gc.ca
|