How a baby can be positioned in the uterus and what can be done in certain cases to ensure a smooth delivery.
This fact sheet describes how a baby can be positioned in the uterus at the end of pregnancy and what can be done in some cases to make delivery as smooth as possible.
Your baby may change positions several times during your pregnancy. This is not very common, however, and is more likely to occur with a second or third baby, since there is more room to move around in the uterus. The baby’s position will always be checked when you arrive at the hospital to ensure that they are still presenting head down.
Head-first presentation
At the end of pregnancy, most babies turn over into the head-down position in anticipation of delivery. This usually happens around the 30 to 35 week mark, but can vary considerably from one pregnancy to the next. In rare cases, babies may turn over as early as 24 weeks or after 36 weeks.
Head-first presentation is the optimal position for a smooth delivery. This presentation has two main variations:
Anterior position
The baby faces the mother’s back with their back pressed against the mother’s belly. In the anterior position, babies can more easily get into the right position to exit through the birth canal.
Posterior position
The baby faces forward with their back pressed against the mother’s spine. Posterior-facing babies need to turn around to get into the best position for delivery.
Most babies are able to do this on their own. Statistics show that 10–35 percent of babies begin labour in the posterior position, but only 5 percent are born in this position.
What happens when your baby stays in the posterior position?
When a baby remains in the posterior position, this may cause problems during delivery. This position prevents the baby from tilting their head forward, so the largest part of the skull has to go through the birth canal first.
Deliveries with a persistent posterior presentation take longer and are more likely to end in an assisted delivery requiring forceps or a vacuum, or in a Csection. During the final stage of labour, the doctor may use their hands or, more rarely, rotational forceps to turn the baby’s head to the anterior position.
Some health care professionals recommend that pregnant women spend 10 minutes a day on all fours during the final weeks of pregnancy. This can help the baby place themself in the anterior position. Some recommend that mothers use the hands and knees position during labour. However, studies have shown that this method is not effective in preventing Csections.
With that in mind, it’s best if mothers change positions regularly throughout labour and prioritize vertical positions such as sitting, standing, or squatting. These positions are effective in advancing labour regardless of the baby’s position.
Breech presentation
 Some babies remain in a heads-up position. This is called a breech presentation.
Some babies remain in a heads-up position. This is called a breech presentation.There are 3 breech variations:
-
Frank breech: Baby’s legs are pointing up with the feet close to the head (see image)
-
Complete breech: Baby’s legs are folded with the feet close to the buttocks
-
Footling breech: One or both of baby’s feet are pointing downwards
If at around the 36th week of pregnancy, your doctor thinks that your baby is in a breech position, they may order an
ultrasound to confirm.
Illustration: Maurice Gervais, From Tiny Tot to Toddler.
External version for breech positioning
If your baby is in a breech position, your doctor may perform a procedure called a version. A version is an external manoeuvre that gently repositions the baby, putting them in a better position for labour and delivery.
During a version, the doctor places their hands on the mother’s belly and gently pushes on the baby. This procedure is always done externally. It can be painful for the mother, especially if it is her first child. A second doctor may be called in to assist and an ultrasound may be performed to facilitate the procedure.
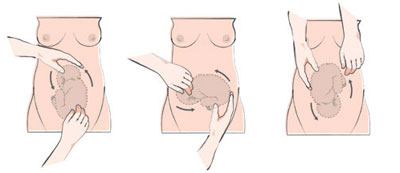
The doctor may also use medication to relax the uterus, making it easier to manipulate. Baby’s heart will be monitored to ensure that it maintains a normal rhythm.
A second ultrasound will confirm whether the version has worked, that is, whether the baby is now in a head-down position. If the version doesn’t work or if your baby flips over again, you can talk to your doctor. They may decide to give it another try. An epidural can improve the chances of success during a second attempt.
After a version, mothers are more likely to give birth vaginally, without a Csection.
In some situations, a version may be contraindicated—for example, if amniotic fluid levels are low. A version may also disrupt the fetal heart rate or induce labour. These situations are rare, but your medical team will still be ready to intervene. Despite these possible complications, a version carries fewer risks than a C-section does.
Images: CHUM Birthing Centre
Can a breech baby be delivered vaginally?
In some cases, breech babies can be delivered vaginally, particularly when the baby is in a frank or complete breech position. Vaginal delivery with breech presentation is also more common in mothers who have previously given birth vaginally. This type of delivery is performed in many hospitals. However, it’s important to assess the situation carefully to ensure the safety of both mother and baby. It’s best to discuss your options with your doctor or midwife.
Transverse presentation
Sometimes a baby will lie horizontally in the uterus. This position is very rare, seen in only about 1 percent of all births. In these cases, the shoulder presents first in the birth canal during a vaginal delivery. Because of the risks this presentation carries, a Csection will be performed.
Face presentation
In 0.2 percent of births, the baby presents face-first, with their head bent back so that the back of the head touches their back. As a result, the chin presents itself first in the birth canal. Vaginal delivery is possible in 60–70 percent of these cases, but forceps may be needed to assist the birth. If labour stops or the baby’s heart rate becomes a concern, a Csection will be performed.
Things to keep in mind
-
Most babies are positioned head down at the end of pregnancy.
-
Breech babies can be repositioned with a manoeuvre called a version.
-
In some cases of breech presentation, a vaginal delivery is possible.
| Scientific review: Roxanne Piché, nursing adviser, Maternal Fetal Medicine Clinic, CHU Sainte-Justine
Research and copywriting: The Naître et grandir team
Updated: October 2021
|
Photo: iStock/RuslanDashinsky
Sources
Note: The links to other websites are not updated regularly, and some URLs may have changed since publication. If a link is no longer valid, please use search engines to find the relevant information.
-
AboutKidsHealth. “Breech and other unusual deliveries.” www.aboutkidshealth.ca
-
Ahmad, Aishah, et al. “Association between fetal position at onset of labor and mode of delivery: a prospective cohort study.” Ultrasound in Obstetrics & Gynecology, vol. 43, no. 2, February 2014, pp. 176–182.
-
Carseldine, Wendy J., et al. “Does occiput posterior position in the second stage of labour increase the operative delivery rate?” Australian and New Zealand Journal of Obstetrics and Gynaecology, vol. 53, no. 3, June 2013, pp. 265–270.
-
CHUM Birthing Centre. www.chumontreal.qc.ca
-
Desbrière, Raoul, et al. “Is maternal posturing during labor efficient in preventing persistent occiput posterior position? A randomized controlled trial.” American Journal of Obstetrics & Gynecology, vol. 208, no. 1, January 2013, pp. 60.e1–8.
-
Doré, Nicole, and Danielle Le Hénaff. From Tiny Tot to Toddler: A practical guide for parents from pregnancy to age two. Quebec City, Institut national de santé publique du Québec. www.inspq.qc.ca
-
Kariminia, Azar, et al. “Randomised controlled trial of effect of hands and knees posturing on incidence of occiput posterior position at birth.” BMJ, vol. 328, 2004.
-
Lande, Laura. A comparison of factors associated with occiput posterior positioning and outcomes for women delivering infants in persistent occiput posterior versus occiput anterior position. Master of Science in Nursing thesis, University of British Columbia, April 2015.
-
Regan, Lesley. Votre grossesse au jour le jour. 2nd ed., Hurtubise, 2010.
|